The fundamentals of aqueous humour dynamics and trabecular meshwork anatomy
Maintenance of normal IOP
A healthy intraocular pressure (IOP) is maintained through a balance between the generation of aqueous humour (AH) within the eye and the drainage of AH from the eye. AH drainage is regulated through two distinct pathways:1,2
The majority (70%-96%) of AH outflow is through the trabecular pathway.3,4
Drainage occurs continuously from the anterior chamber, through the trabecular meshwork (TM), into the Schlemm’s canal (SC) and ultimately into the venous system.1
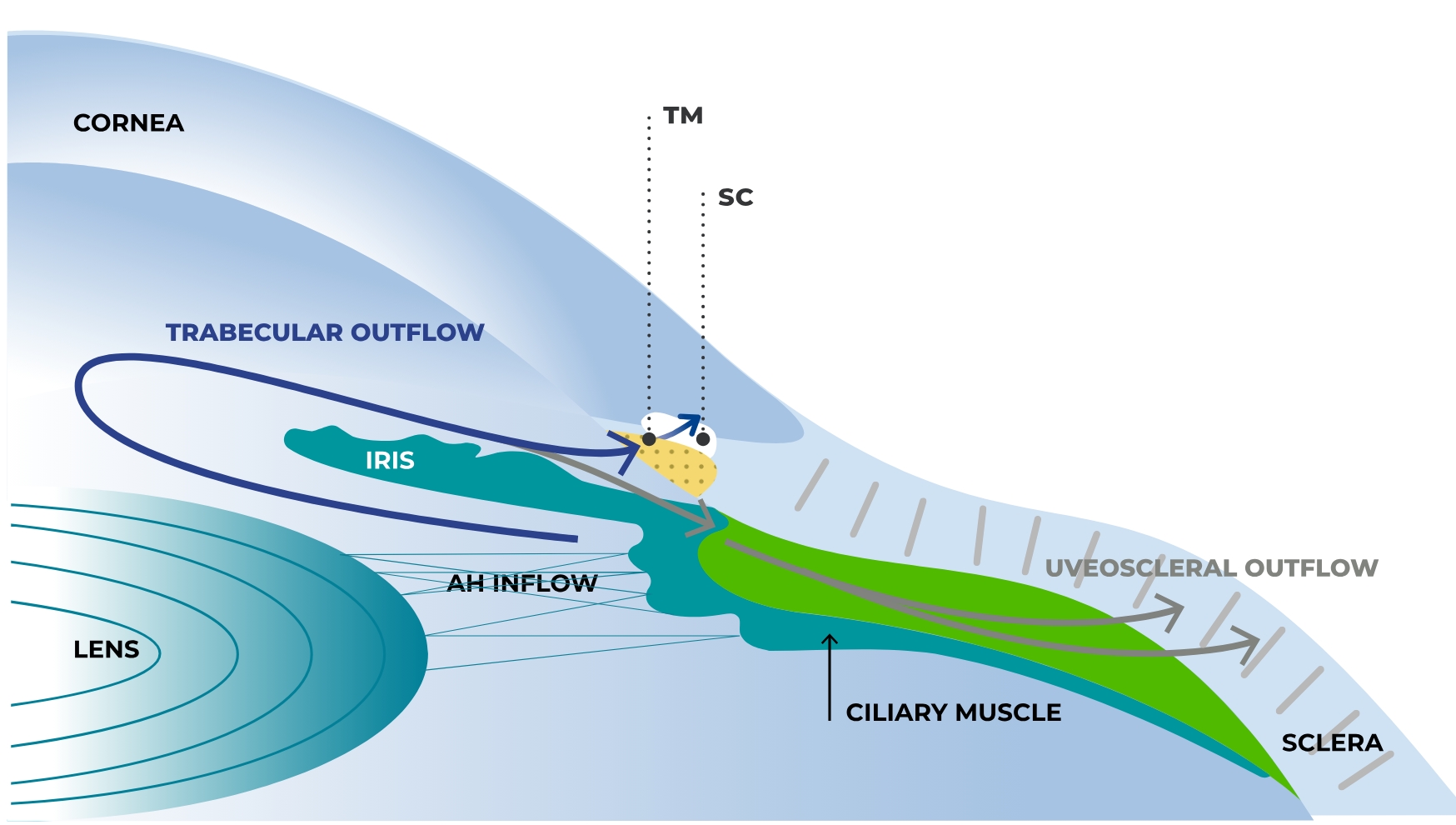
Adapted from Llobet A et al, 20031
The TM and SC are the main sites of outflow resistance.3-6
The TM is a sieve-like structure found in the iridocorneal angle.5,7,8 It acts as a conduit between the anterior chamber (AC) and the SC, and plays a critical role in regulating IOP.3
The TM is composed of multiple layers of extracellular matrix (ECM) covered with endothelial-like TM cells.9 These highly specialised cells perform several functions, including maintenance of AH outflow, elimination of extracellular debris from the AH through phagocytosis, and secretion of ECM proteins and specific enzymes.10,11
- TM cells generate and regulate the majority of outflow resistance to maintain IOP5,10
- IOP is maintained within a normal range in around 90% of people over their lifetime10
- Increased resistance in the trabecular outflow pathway is the main cause of elevated IOP and therefore is implicated as a central underlying cause of primary open-angle glaucoma (POAG)12
In POAG, AH outflow is altered due to changes in the organisation, structure and integrity of the TM tissue, mainly involving the innermost region of the TM, the juxtacanalicular tissue.8,13
Until recently, no medical treatments primarily target TM dysfunction to increase trabecular outflow.14,15*
There remains an unmet medical need in glaucoma management: many patients with glaucoma require at least two different medications to adequately lower IOP16,17 and despite clinical care, disease progression still occurs for a significant proportion of people.18
IOP-lowering agents and primary sites of action 14
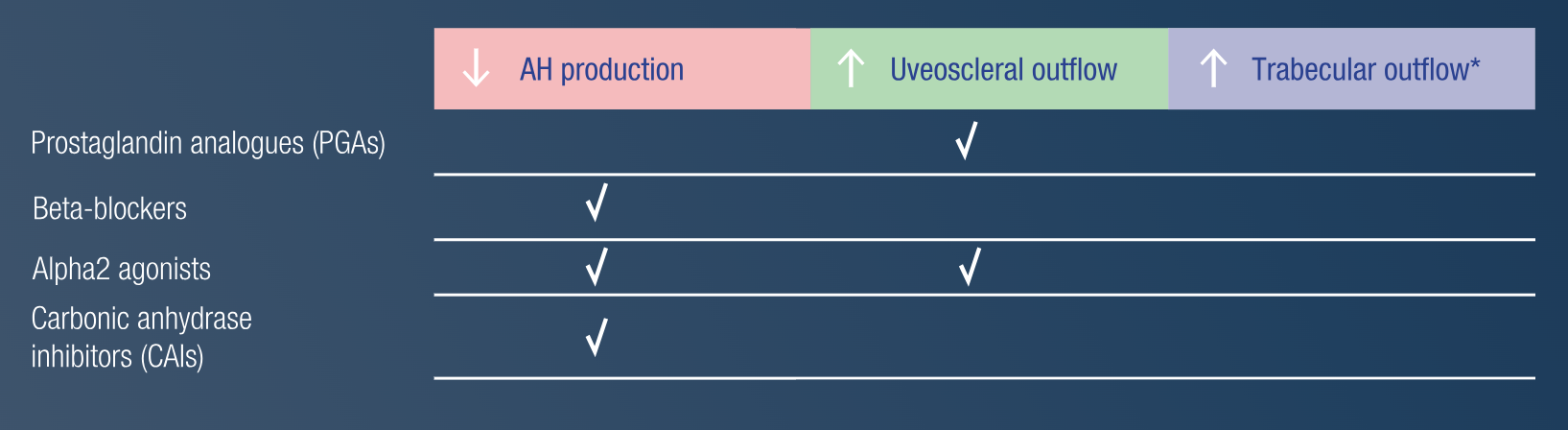
*Cholinergic medications (eg pilocarpine) facilitate AH outflow indirectly by contraction of the ciliary muscle, tension of the scleral spur and traction on the TM.14
Read about innovations in glaucoma management >
References
Llobet A, Gasull X, Gual A. Understanding trabecular meshwork physiology: a key to the control of intraocular pressure? News Physiol Sci 2003;18(5):205-209
Jonas J B, Aung T et al. Glaucoma. Lancet 2017;390(10108):2183-2193
Koga T, Koga T et al. Rho-associated protein kinase inhibitor, Y-27632, induces alterations in adhesion, contraction and motility in cultured human trabecular meshwork cells. Exp Eye Res 2006;82(3):362-370
Park J-H, Chung H W et al. Morphological changes in the trabecular meshwork and Schlemm’s canal after treatment with topical intraocular pressure-lowering agents. Sci Rep 2021;11(1):18169
Goel M, Picciani R G et al. Aqueous humor dynamics: a review. Open Ophthalmol J 2010;4:52-59
McDonnell F, Dismuke W M et al. Pharmacological regulation of outflow resistance distal to Schlemm’s canal. Am J Physiol Cell Physiol 2018;315(1):C44-C51
Buffault J, Brignole-Baudouin F et al. The dual effect of Rho-kinase inhibition on trabecular meshwork cells cytoskeleton and extracellular matrix in an in vitro model of glaucoma. J Clin Med 2022; 11(4)
Buffault J, Labbé A et al. The trabecular meshwork: structure, function and clinical implications. A review of the literature. J Fr Ophtalmol 2020;43(7):e217-e230
Vranka J A, Kelley M J et al. Extracellular matrix in the trabecular meshwork: intraocular pressure regulation and dysregulation in glaucoma. Exp Eye Res 2015;133:112-125
Stamer W D, Clark A F. The many faces of the trabecular meshwork cell. Exp Eye Res 2017;158:112-123
Sun H, Zhu Q et al. Trabecular meshwork cells are a valuable resource for cellular therapy of glaucoma. J Cell Mol Med 2019;23(3):1678-1686
Cela D, Brignole-Baudouin F et al. The trabecular meshwork in glaucoma: an inflammatory trabeculopathy? J Fr Ophtalmol 2021;44(9):e497-e517
Abu-Hassan D W, Acott T S, Kelley M J. The trabecular meshwork: a basic review of form and function. J Ocul Biol 2014;2(1);doi:10.13188/2334-2838.1000017
European Glaucoma Society terminology and guidelines for glaucoma, 5th Edition. Br J Ophthalmol 2021;105(Suppl 1):1
Li T, Chao T et al. The molecular mechanisms of trabecular meshwork damage in POAG and treatment advances. In: Prof. Pinakin Gunvant Gunvant D, ed. Glaucoma – recent advances and new perspectives. Rijeka: IntechOpen, 2022:Ch. 1
Kass M A, Heuer D K et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120(6):701-713
Michelessi M, Lindsley K et al. Combination medical treatment for primary open angle glaucoma and ocular hypertension: a network meta-analysis. Cochrane Database Syst Rev 2018;5(5):CD011366
Saunders L J, Medeiros F A et al. What rates of glaucoma progression are clinically significant? Expert Rev Ophthalmol 2016;11(3):227-234